As of April 2020, everyone with a Medicare card, in Australia, is eligible for Medicare-funded telehealth. That means you can have a consultation with your GP, psychologist and other health providers via video or phone, rather than going in.
This should help with social distancing – a core weapon in our community’s fight to contain this epidemic.
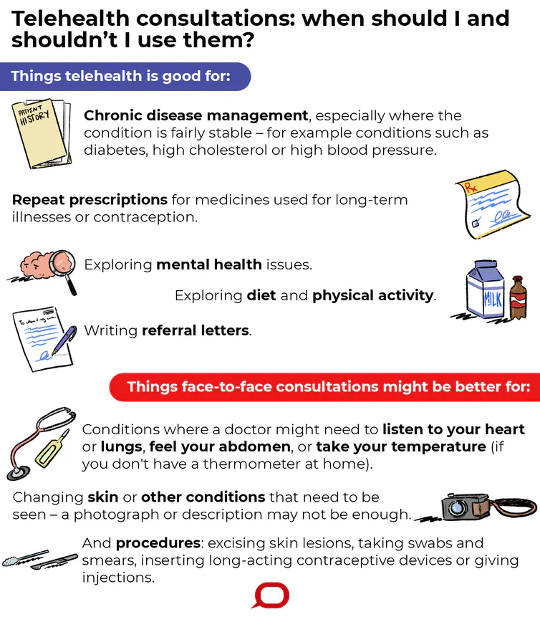
Some but not all health care can safely be shifted online. But it can be difficult to know when it’s OK to skip the in-person visit. Here are some pointers to get you going.
What you can do via telehealth
There’s a saying in medicine that “history is 80% of diagnosis”. By “history”, we mean the things our patients tell us; fortunately, video and telephone connections convey your voices and stories well.
Get The Latest By Email
So for issues where doctors and patients mainly need to speak, and where the risk of serious illness is low, telehealth consults are a good option. Evidence backs this up, finding fairly satisfied doctors and patients – and sometimes even cost or time savings.
The Conversation, CC BY-ND
I’m most comfortable using telehealth with patients I know well, and when we are managing long-standing health issues. For example:
-
routine chronic disease management, especially where the condition is fairly stable – for example conditions such as diabetes, high cholesterol or high blood pressure
-
writing repeat prescriptions for medicines used in long-term illnesses – like the examples above, or tablets for contraception, stomach acid or chronic pain
-
exploring mental health issues
-
discussing diet and physical activity
-
writing referral letters.
Some conditions can also be monitored remotely. In particular, many patients with high blood pressure can safely measure this using a machine at home. This is recommended in blood pressure guidelines, as it’s actually more reliable than clinic readings.
But home blood pressure monitoring won’t be a solution for everyone. It needs careful technique, and also enough money to buy a machine.
Some simple short-term illnesses might also be managed via telehealth, as long as the risk of anything serious going on seems low. Examples could include straightforward urinary tract or upper respiratory tract infections.
But there is a worrisome overlap in symptoms between common viral infections and the early symptoms of COVID-19. Guidelines are being written to help GPs assess, over telehealth, who needs to simply isolate, who needs testing, and who needs to go to hospital.
What you need to see a doctor for
Sometimes a physical examination is important. There are all sorts of presentations in which I might need to listen to your heart or lungs, or feel your abdomen, or take your temperature if you don’t have a thermometer at home. This is especially the case when symptoms are new.
Photographs are tricky. I can’t expect patients to be able to describe or photograph a changing skin lesion well enough for me to make decisions. (Often these are benign, but I’d hate to miss a skin cancer.)
There are procedures that can’t be done via telehealth. Excising skin lesions, taking swabs and smears, inserting long-acting contraceptive devices, giving injections – these simply don’t happen “virtually”.
Particularly important right now are flu vaccinations: while these offer no protection against coronavirus, they may stop the dangerous “double whammy” of getting influenza and coronavirus together.
What you might need to put off
Some routine checkups and screening tests, in low-risk people without symptoms, might simply best be put off until this pandemic settles. But it’s hard to generalise. If in doubt, ask a doctor who knows you well.
Bookings, prescriptions and blood tests
When booking an appointment, don’t simply book a face-to-face appointment out of habit. Hopefully reception staff will offer the telehealth option, but this is all new, and it can’t hurt for you to raise the idea too.
When GPs aren’t sure whether telehealth is appropriate, we can begin with a telehealth conversation, then swap to a traditional consultation if needed.
Prescriptions and blood test or imaging referrals are currently awkward via telehealth. I can mail non-urgent prescriptions and requests to patients, pharmacies or other providers.
For urgent prescriptions, we’re using a messy combination of phone calls, faxes or emails to get instructions to pharmacists quickly, and then mailing the originals.
Fingers crossed, there will soon be reforms allowing purely digital prescribing.
Just an interim measure for the pandemic?
Medicare has previously been very strict about only funding GP consultations when they happen face-to-face. The shift to funding telehealth has been forced by the coronavirus pandemic; so far the government is promising telehealth funding to late September.
Like patients, not all practices are ready for video consultations. Webcams, like facemasks and hand sanitiser, are hard to find. And we’re still learning which video services tick all the boxes for function and privacy.

Doctors, like patients, are still working out how to consult via telehealth. Shutterstock
At a better time in history, we’d confine telehealth consultations to the obviously safe consultations, and do all the other ones face-to-face. But we currently need to balance the risks of forgoing some physical examination and procedures against the risks of potential exposure to coronavirus.
Research evidence on telehealth isn’t much help, because it wasn’t done in the coronavirus era. Instead, we need to be as safe and wise as we can, and learn as we go.
I hope we’ll be able to lay the foundation for telehealth not just as an emergency measure, but as an enduring feature of general practice – complementing rather than replacing face-to-face consultations.
 About the Author
About the Author
Brett Montgomery, Senior Lecturer in General Practice, University of Western Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
books_health









