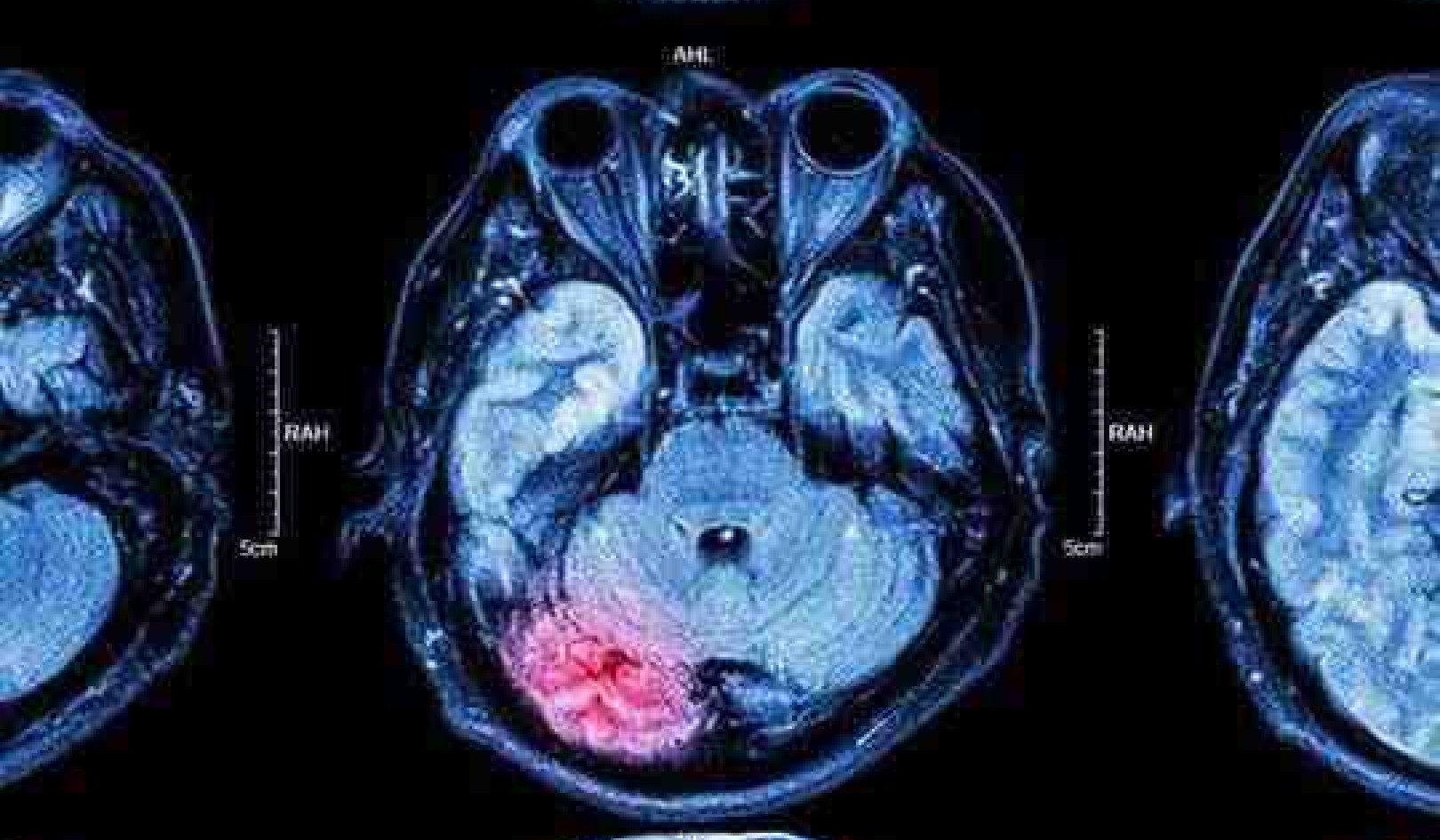
Christoph Burgstedt/ Shutterstock
While our immune system and antibiotics both do a great job of helping us fight life-threatening infections, the emergence of antibiotic resistance is quickly making it more difficult to cure common infections that were once easily treated. Antibiotic resistance happens when bacteria evolve and survive the treatments designed to eliminate them – and then reproduce or pass this resistance on to other bacteria.
Plenty of research is currently taking place to find ways of preventing the spread of antibiotic resistance. But there are still many questions that researchers don’t have answers to. One such question is knowing how resistance evolves inside a person in real-time. Knowing what happens in the body during an infection could help us develop better treatments for antibiotic resistance.
In our recently published study, we investigated the bacterial population in the lungs of an intensive care patient who had a lung infection caused by a common type of bacteria, Pseudomonas aeruginosa. We were able to observe in real-time how both the rapid evolution of antibiotic resistant bacteria, alongside the immune system’s action, were important in determining the outcome of the patient’s infection.
We used a number of techniques and experiments that measured bacterial growth and any changes in antibiotic resistance that happened during the infection. We paired these experiments with genome sequencing techniques to identify changes to the bacterial genetic code. This told us how the bacteria evolves, and whether it evolved antibiotic resistance.
Get The Latest By Email
We also measured the number of immune system molecules present in the lungs which were known to fight against Pseudomonas aeruginosa. Samples from the lungs were analysed every few days – allowing us to capture in high resolution the changes that were taking place. This revealed in unprecedented detail how the immune system played a role in suppressing the antibiotic resistant bacteria that evolved.
We found that the bacteria in the lungs became highly resistant to one of the antibiotics used to eliminate them. These bacteria evolved resistance by mutating and modifying components of their cell wall (the outer layer surrounding the cell). Some bacteria were even found to have modified an entry point in the cell wall used by antibiotics to destroy them. Others were found to have modified a structural element of this layer.
While modifying the entry point massively increased antibiotic resistance, it also made the bacteria less fit. This caused them to grow slower as a result. These highly resistant bacteria rapidly disappeared from the population following the end of antibiotic treatment, replaced by more fit and faster growing relatives.
But the bacteria which only modified a structural element of their cell wall had increased antibiotic resistance – without cost to their survival. In fact, they were able to grow faster. If these bacteria were passed to another person, they would be able to cause infections that are more difficult to treat with antibiotics. These bacteria remained in the lungs – even after their less fit relatives were replaced.
The immune system
Here is where the immune system was really important.
Before the person was treated with antibiotics, we found that the population of bacteria causing the infection had already begun to decline. This showed us that the immune system was doing its job. This also made the antibiotics more successful, as they work better when targeting small bacterial populations.
However, the bacterial infection reappeared around 11 days after it was last detected – and with antibiotic resistant mutants. The first time, the immune system worked together with the antibiotics. This time no new antibiotics were administered, and our research revealed that the immune system was able to fight the infection on its own.
Crucially, this revealed that natural immunity was able to wipe out the population of antibiotic resistance bacteria that emerged following the first course of antibiotic treatment.
We can’t be 100% sure whether the mutant bacteria were or weren’t passed on to other people, but the less time the bacteria are at high levels in the lungs, the less likely it is to be passed on. Such infections can be passed on via a patient coughing and expelling the bacteria from the lungs, and so on.
Our findings suggest that natural immunity can suppress resistance during infection and limit the transmission of resistant strains between patients. In the future, exploiting this link could help us develop new therapeutics to use against harmful bacteria – and may help us better prevent the spread of antibiotic resistant bacteria.![]()
About The Authors
Rachel Wheatley, Postdoctoral Researcher in Bacterial Evolution, University of Oxford and Julio Diaz Caballero, Postdoctoral Researcher in Microbial Genomics, University of Oxford
books_health
This article is republished from The Conversation under a Creative Commons license. Read the original article.