Most vaccines have side-effects and COVID vaccines are no different. The public are being reassured that if they experience a sore arm where the needle went in, or tiredness, a headache, fever or nausea, these are merely signs that the immune system is working as it should. This has left some people wondering: if that’s the immune system doing what it’s supposed to do, does a lack of side-effects mean my immune system hasn’t been primed to protect me?
Rest assured, it means no such thing. The vaccine clinical trials conducted by Pfizer show that 50% of the participants did not experience significant side-effects during the trial, yet 90% of the participants developed immunity against the virus. And the advice on the Moderna vaccine says that common side-effects may be experienced by one in ten people, yet the vaccine protects 95% of those who take it.
This can be explained by considering the way the immune system develops protective immunity against viruses when triggered to do so by a vaccine. Most COVID vaccines, including several that have been authorised, use a viral protein found on the outer envelope of the coronavirus, known as the spike protein, to mimic a natural viral infection and initiate an immune response.
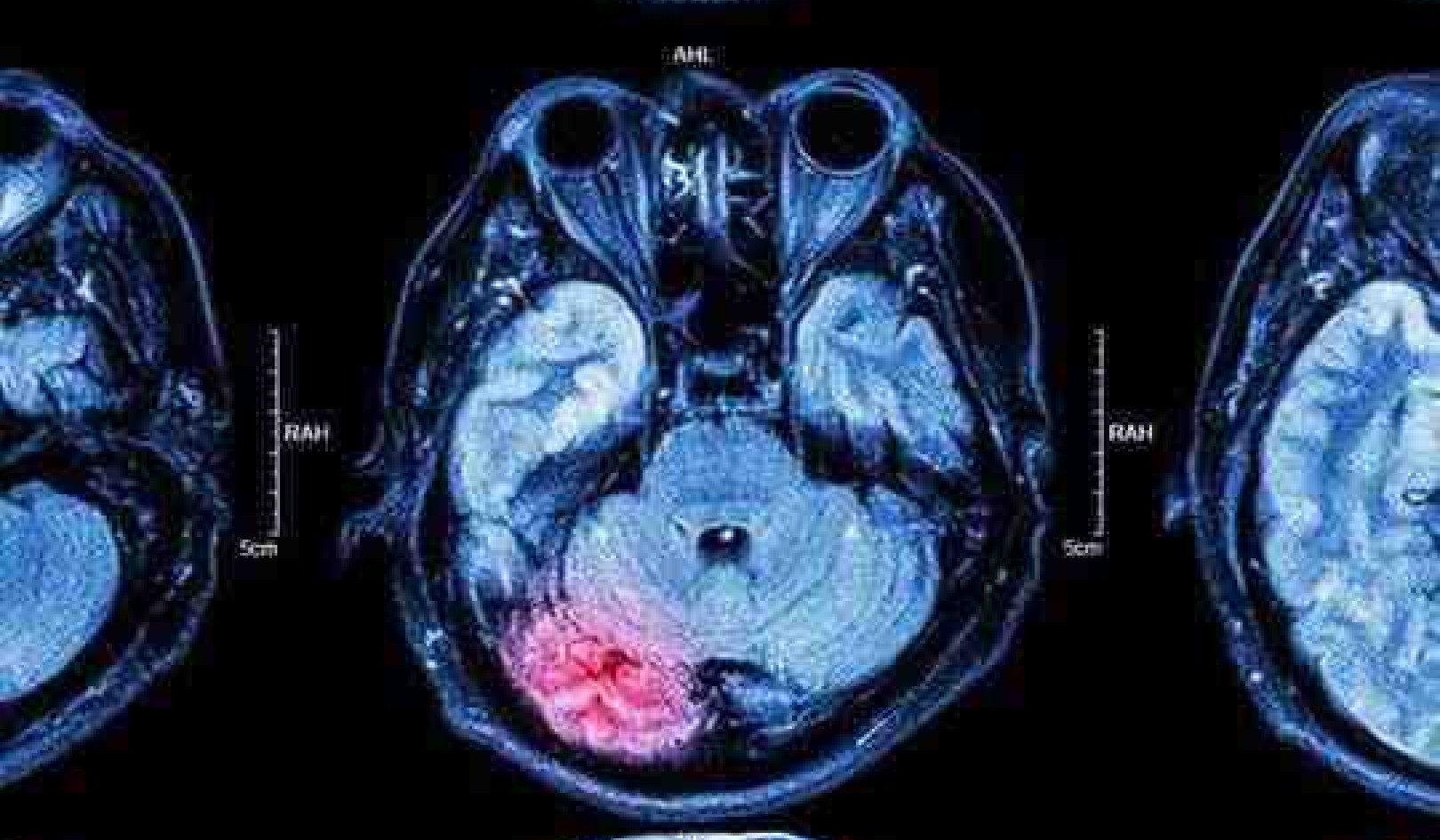
The branch of the immune response known as innate immunity responds almost immediately to the viral spike protein. It launches an attack against it by initiating inflammation, the cardinal signs of which are fever and pain. So it’s the innate immune response that causes the common side-effects that people experience a day or two after they’ve had the jab.
Get The Latest By Email
Innate and adaptive immunity explained.
Long-lasting specific immunity, which is the ultimate goal of any vaccination, is achieved only by activating the second branch of the immune response: adaptive immunity. Adaptive immunity is triggered with the aid of the innate immune components and results in the generation of T cells and antibodies, which protect against infection on subsequent exposure to the virus.
Unlike innate immunity, adaptive immunity can’t initiate inflammation, though recent studies suggest that it can contribute to it significantly. In some people, this inflammatory response by both the innate and adaptive immune systems is exaggerated and manifests as a side-effect. In others, although it is working normally, it is not at levels that can cause noticeable side-effects. Either way, immunity against the virus is established.
What causes a different immune response?
Scientists have noticed that people above the age of 65 are having fewer side-effects to the vaccine. This can be attributed to the gradual age-related decline in immune activity. Although this has can be related to lower antibody levels they still have immunity against the virus.
Sex can also play a role. In a US study, 79% of reports of side-effects were from women. This sex bias could have something to do with testosterone. Testosterone tends to dampen inflammation and hence the side-effects associated with it. Men have more testosterone than women, which might contribute to fewer reports of side-effects in men.
People suffering from chronic inflammatory diseases, such as rheumatoid arthritis, inflammatory bowel disease and multiple sclerosis, who are on immunosuppressive drugs to control their symptoms, may experience fewer side-effects due to a dampened inflammatory response. Although the immune response is dampened, it does not mean that it is nonexistent. In a 2020 study that compared antibody levels in people who were on immunosuppressive drugs to those who were not, it was determined that people on immunosuppressive drugs produced lower levels of antibody but none of them were devoid of antiviral antibodies.
Vaccine side-effects shouldn’t be taken as a measure of the effectiveness of the vaccine. Despite the varied immune response to vaccines, most people achieve immunity against the coronavirus on vaccination, regardless of the presence, absence and severity of side-effects.![]()
About The Author
Veenu Manoharan, Lecturer of Immunology, Cardiff Metropolitan University
books_health
This article is republished from The Conversation under a Creative Commons license. Read the original article.