 Despite recent attempts to retain traditional healing practices in China, modern medicine is supplanting traditional medicine there. Jean-François Chénier
Despite recent attempts to retain traditional healing practices in China, modern medicine is supplanting traditional medicine there. Jean-François Chénier
Most of traditional healing practices are based on intuitive principles of diseases involving the imbalance of elemental qualities.
For the ancient Greeks and Romans, whose systems of traditional healing were accepted in Europe until the scientific revolution, these elements were the four bodily fluids or humours. Each corresponded to the four fundamental elements of the world – earth, water, air and fire.
In traditional Chinese medicine, the elements are wood, fire, earth, metal and water; for the ancient Unani medicine in India, the four humors (akhlaat) are air, earth, fire and water; for Indian Ayurveda medicine, health is the balance of three elemental energies in the universe: air, water and fire.
None of the ideas have any scientific basis.
Get The Latest By Email
With the advent of modern medicine, traditional European practices were relegated to a handful of surviving herbal remedies. Similarly in China, despite recent attempts to retain traditional healing practices, modern medicine is supplanting traditional medicine.
Paradoxically, in Australia and other developed countries there’s increased interest in complementary and alternative medicines, reverting to irrational approaches to health practice, despite people from such countries benefiting most from medicine’s advances.
 Chinese medicinal herbs. Jennifer Yin
Chinese medicinal herbs. Jennifer Yin
The resurgence of interest in traditional Chinese healing in Australia, along with other alternative medicines, is due to rising discontent with conventional medicine; a preference for natural (or gentler) alternatives to pharmaceutical drugs or surgery; desire for greater control over personal health care and the relatively low success rate of conventional medicine in treating conditions, such as chronic pain, for some individuals.
This has led to the recent contentious decision to permit traditional Chinese medicine practitioners to be registered with the new national Chinese Medicine Board of Australia from July this year. The board will be a new member of the Australian Health Practitioner Regulation Agency.
I have argued against the move, along with my colleague Associate Professor Hubertus Jersmann, in articles published today in MJA Insight and the Sydney Morning Herald.
The decision follows Victoria’s move (in 2000) to register traditional Chinese medicine practitioners, which has had a positive impact on tightening standards and dealing with complaints.
Among traditional Chinese medicine practitioners to be registered are those who provide Chinese medical diagnosis, dispense Chinese herbs and perform acupuncture. All three components of this practice have serious flaws, being based on non-existent energies (Yin and Yang), non-existent bodily structures (meridiens) and on principles of disease diagnosis based on the imbalance of five non-existent elements. It is therefore doubtful whether such practitioners are able to make correct and safe diagnoses.
Proponents of traditional medical practices often point out that extracts from animals and plants have been the source of effective remedies in modern medicine. And while pharmacology and medicinal chemistry have enabled this revolution since mid-1800s, only a handful of the extracts used in traditional healing have been proven to contain active principles beneficial for fighting disease. These include about 120 chemical substances out of the thousands of herbal remedies used in traditional medicines.
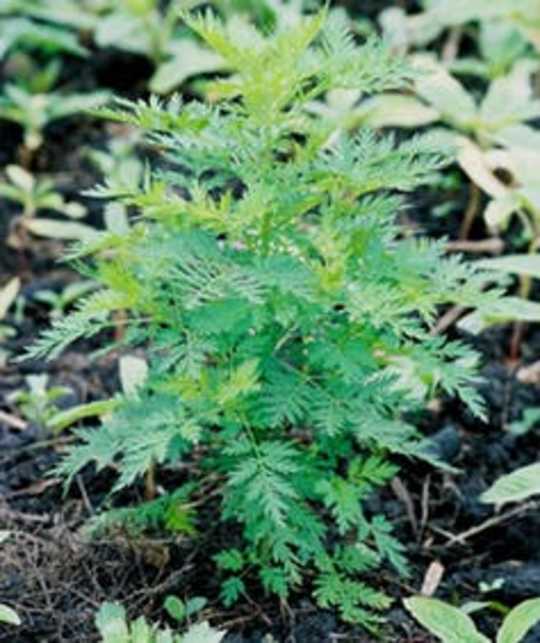 Artemisia annua or qing hao su became incorporated into medicine after it’s anti-malarial activity was proven through research. Scamperdale
Artemisia annua or qing hao su became incorporated into medicine after it’s anti-malarial activity was proven through research. Scamperdale
Take, for instance, qing hao su, a herb used in China for treating fever for over 2,000 years. About 40 years ago, scientific research found that it had specific anti-malarial activity and its active compound, artemesin, was isolated.
In fact, it’s fortunate that most herbal remedies have little acute toxicity. This is due to empirical experience, which over time has selected out those proven to be overtly toxic. But the more subtle, chronic toxicity of herbal remedies remains a serious concern.
Only 6% of plants species have been screened chemically and pharmacologically to identify their active principles. This process, started by modern medicine just over 150 years ago, is continuing with investigations of potential benefits of new therapies often based on a long history of empirical evidence.
This is why research on active chemical principles in herbal remedies showing some potential beneficial effect is fully supported by the Friends of Science in Medicine (FSM), of which I am a founding member.
FSM represents a growing number of medical researchers, clinicians and members of the public concerned by the “current trend which sees government-funded tertiary institutions offering courses in the health care sciences that are not underpinned by sound scientific evidence”. We are worried that this gives unwarranted credibility given to their practitioners and practices, including traditional Chinese medicine.
Even though it falls within traditional Chinese medicine, acupuncture requires separate consideration because, despite being based on a flawed theory of non-existent “meridiens”, it has shown promising effectiveness in some ailments.
 Acupuncture is based on the idea of “meridiens”. aloucha
Acupuncture is based on the idea of “meridiens”. aloucha
But it’s important to remember that despite its popularity, acupuncture has only proven beneficial in alleviating some symptoms of pain and nausea. And the mechanisms by which it appears to work are similar to the physiological processes in the nervous system underlying the placebo effects on pain. Ultimately, research on acupuncture has enabled it to become incorporated in medicine in the few conditions for which it has proven to be effective.
My view, shared by many, is that there’s only one medicine and adjectives such as traditional and “Western” are irrelevant. Rather, medicine is about efficacy and safety, proven through scientific research.
Living in a modern society requires that in matters of health, we unapologetically only accept practices that have undergone the scrutiny of science. And once that criteria is fulfilled, we can accept it as effective medical treatment and teach it in our universities.
Sadly, this is not the case for most traditional Chinese medical practices and practitioners.![]()
About The Author
Marcello Costa, Professor of Neurophysiology, Department of Physiology, Flinders University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
books_disciplines







