For every feeling we experience, there is a lot of complex biology going on underneath our skin.
Pain involves our whole body. When faced with possible threats, the feeling of pain develops in a split second and can help us to “detect and protect”. But over time, our nerve cells can become over-sensitised. This means they can react more strongly and easily to something that normally wouldn’t hurt or would hurt less. This is called “sensitisation”.
Sensitisation can affect anyone, but some people may be more prone to it than others due to possible genetic factors, environmental factors or previous experiences. Sensitisation can contribute to chronic pain conditions like fibromyalgia, irritable bowel syndrome, migraine or low back pain.
But it might be possible to retrain our brains to manage or even reduce pain.
Get The Latest By Email
‘Danger!’
Our body senses possible threats via nerve endings called nociceptors. We can think of these like a microphones transmitting the word “danger” through wires (nerves and the spinal cord) up to a speaker (the brain). If you sprain your ankle, a range of tiny chemical reactions start there.
When sensitisation happens in a sore body part, it’s like more microphones join in over a period of weeks or months. Now the messages can be transmitted up the wire more efficiently. The volume of the danger message gets turned way up.
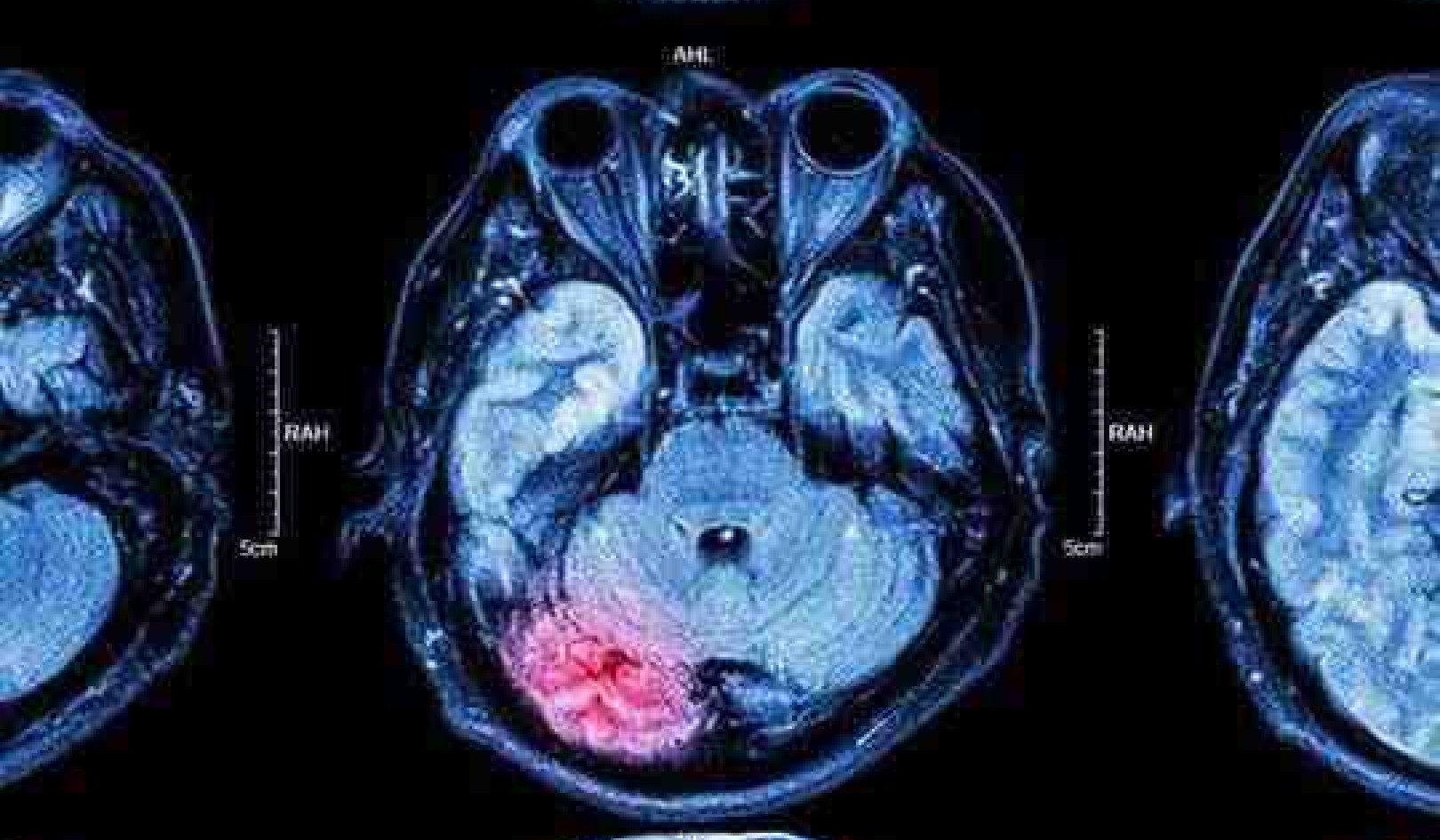
Then, in the spinal cord, chemical reactions and the number of receptors there also adapt to this new demand. The more messages coming up, the more reactions triggered and the louder the messages sent on to the brain.
And sensitisation doesn’t always stop there. The brain can also crank the volume up by making use of more wires in the spinal cord that reach the speaker. This is one of the proposed mechanisms of central sensitisation. As time ticks on, a sensitised nervous system will create more and more feelings of pain, seemingly regardless of the amount of bodily damage at the initial site of pain.
When we are sensitised, we may experience pain that is out of proportion to the actual damage (hyperalgesia), pain that spreads to other areas of the body (referred pain), pain that lasts a long time (chronic or persistent pain), or pain triggered by harmless things like touch, pressure or temperature (allodynia).
Because pain is a biopsychosocial experience (biological and psychological and social), we may also feel other symptoms like fatigue, mood changes, sleep problems or difficulty concentrating.
Neuroplasticity
Around the clock, our bodies and brain are constantly changing and adapting. Neuroplasticity is when the brain changes in response to experiences, good or bad.
Pain science research suggests we may be able to retrain ourselves to improve wellbeing and take advantage of neuroplasticity. There are some promising approaches that target the mechanisms behind sensitisation and aim to reverse them.
One example is graded motor imagery. This technique uses mental and physical exercises like identifying left and right limbs, imagery and mirror box therapy. It has been tested for conditions like complex regional pain syndrome (a condition that causes severe pain and swelling in a limb after an injury or surgery) and in phantom limb pain after amputation. Very gradual exposure to increasing stimuli may be behind these positive effects on a sensitised nervous system. While results are promising, more research is needed to confirm its benefits and better understand how it works. The same possible mechanisms of graded exposure underpin some recently developed apps for sufferers.
Exercise can also retrain the nervous system. Regular physical activity can decrease the sensitivity of our nervous system by changing processes at a cellular level, seemingly re-calibrating danger message transmission. Importantly, exercise doesn’t have to be high intensity or involve going to the gym. Low-impact activities such as walking, swimming, or yoga can be effective in reducing nervous system sensitivity, possibly by providing new evidence of perceived safety.
Researchers are exploring whether learning about the science of pain and changing the way we think about it may foster self-management skills, like pacing activities and graded exposure to things that have been painful in the past. Understanding how pain is felt and why we feel it can help improve function, reduce fear and lower anxiety.
But don’t go it alone
If you have chronic or severe pain that interferes with your daily life, you should consult a health professional like a doctor and/or a pain specialist who can diagnose your condition and prescribe appropriate active treatments.
In Australia, a range of multidisciplinary pain clinics offer physical therapies like exercise, psychological therapies like mindfulness and cognitive behavioural therapy. Experts can also help you make lifestyle changes to improve sleep and diet to manage and reduce pain. A multi-pronged approach makes the most sense given the complexity of the underlying biology.
Education could help develop pain literacy and healthy habits to prevent sensitisation, even from a young age. Resources, such as children’s books, videos, and board games, are being developed and tested to improve consumer and community understanding.
Pain is not a feeling anyone should have to suffer in silence or endure alone.
About the Author
![]()
Joshua Pate, Senior Lecturer in Physiotherapy, University of Technology Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
books_disease