- Home
-
Home & Garden
- Food & Nutrition
Blood test checks to see if cancer treatment is working
- National University of Singapore
- Read Time: 6 mins
Researchers have created a new blood test that can tell doctors whether their patient’s cancer treatment is working, within one day after the start of the treatment.
This will significantly speed up the evaluation process and enable doctors to make adjustments to the treatment plan, if necessary, to improve patients’ chances of recovery.
Unlike conventional chemotherapies that interfere with all rapidly dividing cells and can cause widespread damage to cells, targeted medicines attack specific molecules that instruct cancer cells to grow and spread and in turn, block the abnormal growth of the cancer. Despite the specific nature of targeted drugs, current clinical evaluation of their treatment in solid tumors primarily relies on either tumor volumetric imaging, which is insensitive and delayed, or invasive tissue biopsies.
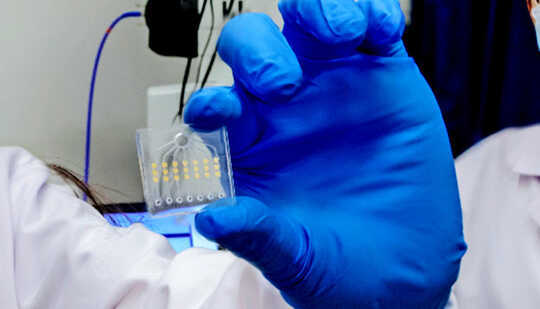
Shao Huilin and her research team from the biomedical engineering department and Institute for Health Innovation & Technology (iHealthtech) at the National University of Singapore (NUS) have developed a technology that is accurate, less invasive, and significantly brings forward the evaluation window, by using liquid biopsies.
The technique, termed extracellular vesicle monitoring of small-molecule chemical occupancy and protein expression (ExoSCOPE), is the first of its kind in the world. It takes advantage of extracellular vesicles (EVs) secreted by cancer cells and circulating in blood as a reflective indicator of drug effectiveness in solid tumors.
Get The Latest By Email
“Conventional procedures such as tumor imaging are not only expensive but also delayed. For these methods, treatment effectiveness can only be determined after weeks. Using the ExoSCOPE, we can directly measure the outcomes of drug effectiveness within 24 hours of treatment initiation. This will significantly reduce the time and cost for cancer treatment monitoring,” says Shao.
“This method requires only a tiny amount of blood sample for the analysis and each test takes less than one hour to complete. So, it is less invasive and yet more informative. In this way, doctors could monitor a patient’s response to treatment more regularly during the course of the treatment, and make timely adjustments to customize the treatment for better outcomes.”
To achieve sensitive and rapid analysis of drug efficacy through blood samples, the researchers developed the ExoSCOPE as an integrated nanotechnology platform. It measures EVs, which are membrane vesicles of dimension at least a hundred times smaller than the diameter of human hair and invisible under conventional light microscopy. During successful cancer treatment, when a targeted cancer drug attaches to a cancer cell and interferes with tumor growth, the treated cell will release into the bloodstream EVs containing the drug.
The ExoSCOPE platform harnesses a complementary approach of chemical biology and sensor development to measure these delicate drug changes in EVs.
“Current technologies to measure drug–target interactions require complex processing and invasive tissue biopsies, limiting their clinical utility for cancer treatment monitoring. By using specially designed chemical probes, our platform is highly sensitive in capturing and labeling EVs in a small blood sample in order to assess drug-target interactions,” says Sijun Pan, a research fellow from NUS iHealthtech, and co-first author of the study.
“The ExoSCOPE sensor contains millions of gold nanorings to capture the EVs and amplify their drug labeling signals to induce strong light signals. These light signals are then processed to give a readout to indicate drug effectiveness,” says co-first author Zhang Yan, a doctoral student from the biomedical engineering department and iHealthtech.
Using the developed ExoSCOPE platform, the team collected information on different types of EVs and their drug changes, when treated with various targeted therapies. The platform not only identifies cancer-released EVs, but also monitors their drug dynamics over time to accurately distinguish treatment sensitivity and resistance.
“Existing blood pharmacokinetic or pharmacodynamic approaches measure the total drug concentration in blood. This ensemble information does not reflect drug efficacy in tumors. The ExoSCOPE, however, measures drug changes in cancer-released EVs to accurately reflect tumor treatment responses,” explains Shao.
In a clinical trial involving 163 blood samples from 106 patients, the ExoSCOPE has shown encouraging results on lung cancer patients to enable timely evaluation of patients’ targeted treatment outcomes. Compared against the gold standard of tumor volumetric imaging, which was performed at the end of the entire treatment regimen, the ExoSCOPE achieved an accuracy rate of 95%, but within 24 hours of treatment initiation.
This technique’s superior analytical performance paves the way for the use of blood-borne EVs for monitoring different interactions between drugs and protein targets in the human body.
“The ExoSCOPE presents a paradigm shift in blood-based drug evaluation for targeted drug selection and real-time treatment monitoring,” says Shao. “The technique can also empower the clinical community to make more timely treatment decisions.”
The nine-member team took two years (from 2019 to 2021) to develop and validate the ExoSCOPE platform. Their next challenge is to expand the platform to measure the efficacy of different drugs and apply the technology to a spectrum of diseases from cancers to cardiovascular and neurological disease. A patent has been filed for ExoSCOPE and the research team hopes to bring this technology to market in the next three years.
“I hope our technology can contribute towards personalized treatment, to guide the selection, dosage, and duration of different treatments, and improve treatment outcomes,” says Shao.
The research appears in the journal Nature Nanotechnology.
Source: National University of Singapore
About The Author
National University of Singaporebooks_health
LATEST ARTICLES

Volunteering in Late Life: A Shield Against Cognitive Decline and Dementia
Tuesday, 25 July 2023 16:09Volunteering in late life may be more than just a noble act of giving back to the community; it could be a critical factor in safeguarding the brain against cognitive decline and dementia.
How Injuries Change Our Brain and How We Can Help It Recover
Monday, 07 June 2021 08:07Injury to the adult brain is all too common. A brain injury will often show up on brain scans as a well-defined area of damage. But often the changes to the brain extend far beyond the visible...

Fact or Fiction: Debunking 4 Common Myths About Ticks
Thursday, 15 April 2021 07:10Blooming flowers, chirping birds and long-awaited rays of sunshine: The first signs of spring are often greeted with joy. But soon comes the realization that with warm weather comes ticks.

4 Steps to Making Your Home a Sanctuary of Love and Joy using Space Clearing
Thursday, 06 May 2021 00:51Have you ever walked into an empty room and immediately sensed that the atmosphere was laced with tension? You may have had no idea what occurred there prior to your arrival, yet you somehow knew...

What Actually Is Catnip and Is It Safe For My Cat?
Monday, 24 May 2021 08:28There are many valid theories to explain the global appeal of cats, including our obsession with watching videos of them online. In terms of cats’ pure entertainment value, however, our...

Baby Bees Love Carbs – Here's Why That Matters
Tuesday, 20 April 2021 08:05Wild bees are essential for sustaining the landscapes we love. A healthy community of wild pollinators ensures that most flowering plants have an A-team pollinator species and a reserve bench of...
New Attitudes - New Possibilities
InnerSelf.com | ClimateImpactNews.com | InnerPower.net
MightyNatural.com | WholisticPolitics.com | InnerSelf Market
Copyright ©1985 - 2021 InnerSelf Publications. All Rights Reserved. - Food & Nutrition




