 A report found that 90% of morbidly obese patients admitted to intensive care needed a ventilator. Patrik Slezak/ Shutterstock
A report found that 90% of morbidly obese patients admitted to intensive care needed a ventilator. Patrik Slezak/ Shutterstock
As worldwide coronavirus-related deaths tip a quarter of a million, a concerning trend is surfacing in the medical literature: high rates of obesity in groups of patients with severe or life-threatening COVID-19.
A recent report from New York shows more than two in every five people requiring a breathing tube were obese. A report from one intensive care unit in France found almost 90% of morbidly obese patients admitted required mechanical ventilation compared to less than half of those with lower body weight.
There are several reason why patients with obesity admitted to intensive care with COVID-19 may require invasive ventilation.
Higher levels of fat in the chest and belly put pressure on the lungs, making it difficult for people with obesity to fill them to capacity under normal circumstances. This reduced breathing capacity may add to respiratory distress in patients with COVID-19.
Get The Latest By Email
Carrying extra weight also means there is higher oxygen demand. Some patients with obesity might breathe too shallowly or too slowly to provide enough oxygen to the body, and some may intermittently cease breathing altogether.
Both of these factors already put strain on the heart and lungs, and may worsen COVID-19 symptoms. But they don’t seem to entirely explain the unexpectedly high rates of obesity in very sick coronavirus infected patients. This suggests that there may be other factors at play which are unique to this virus.
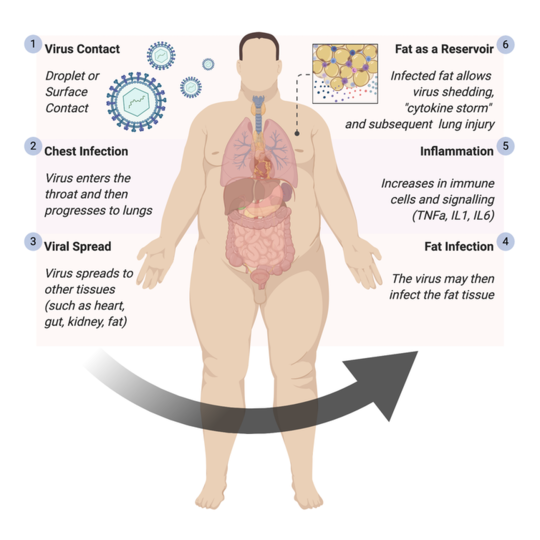
In a recent review paper, we looked at why patients with obesity are at higher risk of severe or life-threatening COVID-19 infections. Based on our findings, we believe fat tissue is a potential source of unchecked inflammation which could cause damage to organs, including the lungs, as a result of COVID-19.
People with obesity are commonly shown to have an unbalanced or inflamed immune system. Their blood often has higher levels of several inflammatory signals which are similar to COVID-19 responses in the body. This may mean their immune systems are more likely to overreact to a coronavirus infection.
Fat tissue also acts as a vast reservoir for a range of immune cells, including macrophages and T cells. Macrophages devour infectious agents (such as bacteria and viruses) and present the leftovers to T cells, who alert the body of infection.
 Fat tissue can act as a reservoir for immune cells. Paul MacDaragh Ryan/ Noel Caplice, Author provided
Fat tissue can act as a reservoir for immune cells. Paul MacDaragh Ryan/ Noel Caplice, Author provided
Data from Wuhan, China indicates that the body’s immune signal response is higher in people with severe forms of COVID-19. This reaction is referred to as a “cytokine storm”.
Cytokines act as “messengers” that tell other immune cells about potential threats and trigger inflammation (often in the form of a fever or swelling) in order to destroy the pathogen. But sometimes the immune system overreacts, releasing too many cytokines (a “cytokine storm”).
After becoming infected with coronavirus, an obese person’s body may activate the large fat-dwelling reservoir of immune cells, which can cause excessive swelling and inflammation. This disproportionate activation of the immune system can cause damage in organs, including the lungs.
At day seven to ten of COVID-19, the patient often either begins to improve or can take a turn for the worse. This delayed deterioration suggests that the true harm caused by COVID-19 may be caused by the cytokine storm, rather than the infection itself.
Because fat tissue stores a large reservoir of immune cells, people with obesity may be more likely to suffer a cytokine storm reaction from COVID-19. This would result in damage to the lungs, severe respiratory distress or even death.
There is currently no approved treatment or cure for COVID-19. Doctors are primarily focusing on keeping patients oxygenated and hydrated.
Targeted immunosuppressive drugs (which reduce the strength of the body’s immune system) may be particularly beneficial for patients with severe infections and trials are currently underway.
However, researchers have also seen deficiencies of specific subpopulations of T cells in severe disease. Therefore, non-targeted immunosuppressive medicines could potentially worsen symptoms by further dampening the immune response.
Several additional inflammatory messengers, such as TNFa, may be worth targeting at different stages of the disease. Testing is ongoing for a number of drugs, with more than 600 clinical trials currently underway. But it may be months before any immune therapies are approved and none of these drugs will be a cure.
People with obesity should take extra measures to protect themselves from getting COVID-19, including following social distancing measures. Public health attention should also be drawn to underpriviledged, overcrowded neighbourhoods where poor diet and obesity often coexist. The threshold for escalating intensive treatment should be lowered for subjects with obesity to prevent severe infection.![]()
About The Author
Paul MacDaragh Ryan, Junior Doctor (Academic Track Intern), University College Cork and Noel Caplice, , University College Cork
This article is republished from The Conversation under a Creative Commons license. Read the original article.
books_health







