
A COVID-19 patient is connected to life-sustaining devices at Mount Sinai South Nassau Hospital in Oceanside, New York on April 14, 2020. Jeffrey Basinger/Newsday via Getty Images
The COVID-19 pandemic has thrust the obesity epidemic once again into the spotlight, revealing that obesity is no longer a disease that harms just in the long run but one that can have acutely devastating effects. New studies and information confirm doctors’ suspicion that this virus takes advantage of a disease that our current U.S. health care system is unable to get under control.
In most recent news, the Centers for Disease Control and Prevention reports that 73% of nurses who have been hospitalized from COVID-19 had obesity. In addition, a recent study found that obesity could interfere with the effectiveness of a COVID-19 vaccine.
Obesity correlates with a dulled immune response to COVID-19, and researchers worry that it might also blunt vaccine efficacy too. https://t.co/lRcNupif1P— Nature News & Comment (@NatureNews) October 25, 2020
I am an obesity specialist and clinical physician working on the front lines of obesity in primary care at the University of Virginia Health System. In the past, I often found myself warning my patients that obesity could take years off their life. Now, more than ever, this warning has become verifiable.
Get The Latest By Email
More damage than believed
Initially physicians believed that having obesity increased only your risk of getting sicker from COVID-19, not your chance of being infected in the first place. Now, newer analysis shows that not only does obesity increase your risk of being sicker and dying from COVID-19; obesity increases your risk of getting infected in the first place.
In March 2020, observational studies noted hypertension, diabetes and coronary artery disease as the most common other conditions – or co-morbidities – in patients with more severe COVID-19 disease. But it was the editors of Obesity journal who first raised the alarm on April 1, 2020 that obesity would likely prove to be an independent risk factor for more severe effects of COVID-19 infection.
Additionally, two studies including nearly 10,000 patients have shown that patients who have both COVID-19 and obesity have a higher risk of death at days 21 and 45 compared to patients with a normal body mass index, or BMI.
And a study published in September, 2020 reported higher rates of obesity in COVID-19 patients who are critically ill and require intubation.
It is becoming overwhelmingly evident from these studies and others that those with obesity are facing a clear and present danger.
Stigma and lack of understanding
Obesity is an interesting disease. It is one that many physicians talk about, often in frustration that their patients cannot prevent or reverse it with the oversimplified treatment plan that we have been taught in our initial training; “Eat less and exercise more.”
It is also a disease that causes problems physically, such as sleep apnea and joint pain. It also affects one’s mind and spirit due to societal and medical professionals’ bias against those with obesity. It can even adversely affect the size of your paycheck. Can you imagine the outcry if the headline read “Patients with high blood pressure earn less”?
We doctors and researchers have understood for quite some time the long-term consequences of excess weight and obesity. We currently recognize that obesity is associated with at least 236 medical diagnoses, including 13 types of cancer. Obesity can decrease one’s lifespan by up to eight years.
Despite knowing this, U.S. physicians are not prepared to prevent and reverse obesity. In a recently published survey, only 10% of medical school deans and curriculum experts feel that their students were “very prepared” in regards to obesity management. Half of the medical schools responded that expanding obesity education was a low priority or not a priority. An average of 10 hours total was reported as dedicated to obesity education during their entire training in medical school.
And doctors sometimes don’t know how or when to prescribe medications for patients with obesity. For example, eight FDA-approved weight loss medications are on the market, but only 2% of eligible patients receive prescriptions for them from their physicians.
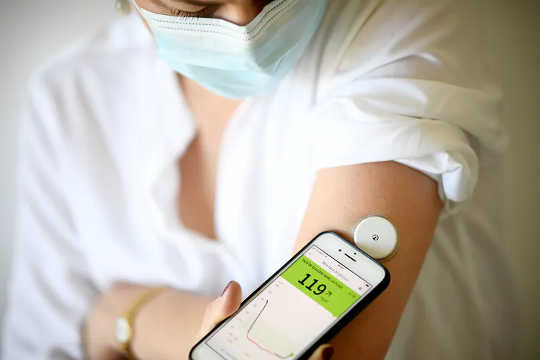 A woman measures her blood sugar level during lockdown in Paris in March 2020. Photo by Franck Fife/AFP via Getty Images
A woman measures her blood sugar level during lockdown in Paris in March 2020. Photo by Franck Fife/AFP via Getty Images
What goes on in the body
So, here we are, with a collision of the obesity epidemic and the COVID-19 pandemic. And a question I find patients asking me more and more: How does obesity create more severe disease and complication from COVID-19 infection?
There are many answers; lets start with structure.
Excess adipose tissue, which stores fat, creates a mechanical compression in patients with obesity. This limits their ability to take in and completely release a full breath of air.
Breathing takes more work in a patient with obesity. It creates restrictive lung disease, and in the more serious cases, lead to hypoventilation syndrome, which can cause a person to have too little oxygen in their blood.
And then there is function. Obesity results in an excess of adipose tissue, or what we colloquially call “fat.” Over the years, scientists have learned that adipose tissue is harmful in and of itself. One may say that adipose tissue acts as an endocrine organ all its own. It releases multiple hormones and molecules that lead to a chronic state of inflammation in patients with obesity.
When the body is in a constant state of low-grade inflammation, it releases cytokines, proteins that fight inflammation. They keep the body on guard, simmering and ready to fight disease. That’s all well and good when they are kept in check by other systems and cells. When they are chronically released, however, an imbalance can occur that causes injury to the body. Think of it like a small but contained wildfire. It’s dangerous, but it’s not burning the entire forest.
COVID-19 causes the body to create another cytokine wildfire. When a person who is obese has COVID-19, two small cytokine wildfires come together, leading to the raging fire of inflammation that damages the lungs even more so than patients with normal BMI.
Additionally, this chronic state of inflammation can lead to something called endothelial dysfunction. In this condition, instead of opening up, blood vessels close down and constrict, further decreasing oxygen to the tissues.
In addition, increased adipose tissue may have more ACE-2, the enzyme that allows the coronavirus to invade cells and begin to damage them. A recent study has shown an association of increased ACE-2 in adipose tissue rather than lung tissue. This finding further strengthens the hypothesis that obesity plays a major role in more serious COVID-19 infections. So in theory, if you have more adipose tissue, the virus can bind to and invade more cells, causing higher viral loads that stay around longer, which can make the infection more severe and prolong recovery.
ACE-2 can be helpful in counteracting inflammation, but if it otherwise bound to COVID-19, it cannot assist with this.
The novel SARS COVID-19 virus has forced the medical profession to face the reality that many U.S. physicians inherently know. When it comes to prevention of chronic diseases such as obesity, the U.S. health care system is not performing well. Many insurers reward physicians by meeting metrics of treating the effects of obesity rather than preventing it or treating the disease itself. Physicians are reimbursed, for example, for helping patients with Type 2 diabetes to attain a certain A1C level, or a set blood pressure goal.
I believe is time to educate physicians and provide them with resources to combat obesity. Physicians can no longer deny that obesity, one of the strongest predictors for COVID-19 and at least 236 other medical conditions, must become public enemy number one.
About the Author
Cate Varney, Clinician Physician, University of Virginia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
books_nutrition







