
British broadcaster Jeremy Paxman has revealed he is one of more than 10 million people living with Parkinson’s disease worldwide. It is the fastest growing neurological condition in terms of diagnosis and cases that lead to disability and death.
Although there is no cure yet, treatments for the disease have come a long way since it was first discovered over 200 years ago. People with Parkinson’s don’t have enough of the chemical dopamine, because some of the nerve cells that make it have died. Dopamine allows messages to be sent to the parts of the brain that co-ordinate movement.
We like to think of the management of Parkinson’s as a table that rests on four legs. There are drugs that replace the missing dopamine or mimic its effects; there is deep brain surgery; lots of different kinds of care; and then there is the importance of keeping patients and their families well informed and engaged.
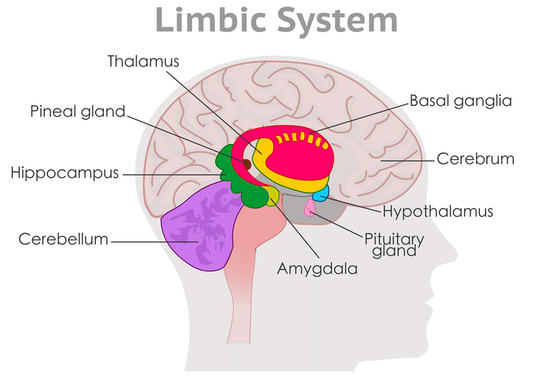
Parkinson’s results from the deterioration of neurons in a part of the brain called the basal ganglia – a group of nuclei deep beneath the cerebral cortex (or outer layer of the brain). These neurons are responsible for processing information on movement and fine tuning activity as well as in a variety of cognitive and emotional functions.
A reduction in dopamine causes a variety of motor symptoms including tremors, rigid limbs and a general slowing of movement. Dopamine deficiency also leads to a wide range of non-motor symptoms – which may be less visible but are still severely debilitating – such as cognitive decline, depression, pain, urinary incontinence and constipation.
Get The Latest By Email
The history of Parkinson’s
Parkinson’s disease was first defined as a “shaking palsy” in 1817 by James Parkinson. Half a century later, in 1872, the Parisian neurologist Jean-Martin Charcot coined the term Parkinson’s disease.
Though Parkinson was the first to describe the disease in modern medicine, Charcot and his colleagues revolutionised treatments in the mid-19th century.. Parkinson was a proponent of blood-letting from the neck, in a bid to siphon off inflammatory pathogens and prevent them from reaching the brain. But Charcot and his colleagues favoured pharmaceutical approaches centred around anticholinergic drugs, which block the action of a neurotransmitter called acetylcholine. Anticholinergics are still in use today.
Around the same time, a host of other treatments were being explored at a hospital in Paris. Hyoscyamine, a plant-derived medication, was put in bread and fed to patients. Other medications, such as a derivative of quinine, were mixed with a syrup of orange rinds.
Charcot also claimed to see the symptoms of patients with Parkinson’s improving when travelling by train and horse-carriage. He became a proponent of vibration therapy, where patients’ bodies and heads were shaken vigorously by a rigged motor.
Modern treatments
Modern treatments can be divided into pharmaceutical and surgical interventions, as well as a wide range of non-pharmacological interventions.
There are six main classes of pharmaceutical treatments.
One of these, known as dopamine therapy, includes the mainstay drug levodopa. These drugs provide an external source of dopamine, acting as a replacement in depleted areas. Another type, called dopamine agonists, mimic the action of dopamine. This allows neurons to maintain communication.
Other types of drugs try to fight the source of the problem, either by preventing the breakdown of dopamine or by increasing its production.
Surgical treatments
Surgery for Parkinson’s, and a host of additional neurological conditions, was popularised at the start of the 20th century. Surgery involved either removing an area of the brain – such as the cerebral cortex – or electrically ablating (using electricity to create targeted burns in specific areas of the brain) other areas. In the 1940s, these kinds of procedures were the primary evidence used to pinpoint the exact location of the disease – the basal ganglia.
Modern surgical techniques, such as deep brain stimulation, target the same area.
Thin wires are threaded deep into the brain, with the tips placed in specific regions of the basal ganglia. The wires are manoeuvred around the exterior of the skull and weaved under the muscles of the neck into a pacemaker-like generator box sitting under the skin in the upper chest.
Wireless control of the generator allows pulses of electricity to be delivered to the part of the brain where the disease occurs. Similarly to a heart pacemaker, these electrical pulses are used to regulate brain activity. Surgery like this provides symptomatic relief, but doesn’t stop disease progression.
Future treatments
Many studies are underway to find new therapies. A variety of medications are being tested, from stem cell treatments to probiotics and some are even testing the potential to use hypoxia – limiting people’s oxygen levels.
Many new trials are focusing on a specific protein, called alpha-synuclein, which is affected by the deterioration of the neurons that causes Parkinson’s. The hope is that targeting the protein could halt the progression of disease.
Stimulation techniques using vibrations are beginning to make a comeback in modern medicine too, although the evidence to support them is still in its early days.
Parkinson’s is well known for being different in every patient, making it a good candidate for personalised medicine – tailoring care to suit the individual. Recent research has shown exercise can help to suppress the motor symptoms of Parkinson’s disease, much like a drug. There’s some initial evidence to suggest it may even help to slow down the progression of Parkinson’s.
People are beginning to acknowledge the importance of a holistic approach, by focusing on treating the patient themselves and not just the disease. Such treatments involve physical, speech and cognitive behavioural therapies. Though these therapies don’t alter the disease progression, by targeting symptoms specific to patients, they can substantially increase their quality of life.
About The Author
This article orginally appeared on The Conversation







