 Here’s what’s happening in your body if you’re feeling faint. William Moss/Shutterstock.com
Here’s what’s happening in your body if you’re feeling faint. William Moss/Shutterstock.com
Maybe it’s a bride standing in a hot chapel, or an exhausted runner after a race. It could be someone watching a medical procedure on television or a donor at a blood drive.
Maybe you’ve even experienced it yourself. You start to feel lightheaded, your stomach may hurt, your palms are sweaty, your vision closes in, your ears start to ring …. Then you wake up on the floor, staring up the ceiling, and realize you’ve fainted. What happened?
Fainting – or what medics more technically call syncope – can be caused by a number of factors. Ultimately it comes down to not enough blood getting to your brain.
Sufficient blood pressure is necessary in order to deliver blood – and therefore oxygen – to all of the tissues in your body. The brain, which when you’re sitting or standing is above the level of your heart, especially relies on sufficient pressure to overcome gravity and drive blood up to your head.
Get The Latest By Email
So what can interrupt that process and cause you to hit the deck before you even know what’s going on?
Nerve signals at odds
 The vagus nerve helps carry out a number of unconscious actions as part of the autonomic nervous system. Alila Medical Media/Shutterstock.com
The vagus nerve helps carry out a number of unconscious actions as part of the autonomic nervous system. Alila Medical Media/Shutterstock.com
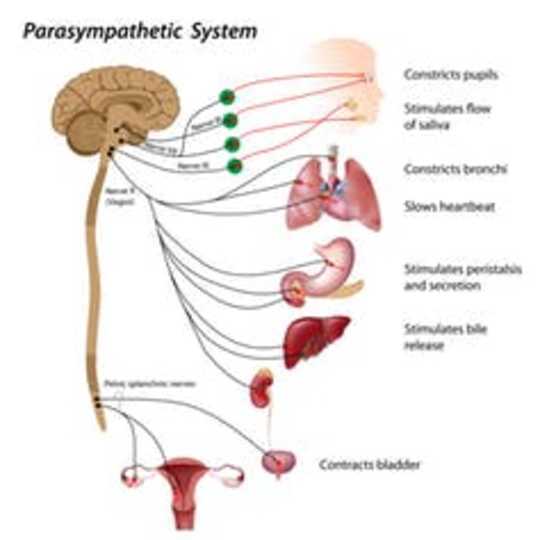
By far the most common trigger for fainting is a drop in blood pressure due to a strong vasovagal response. This reflex is named after the vagus nerve, which runs from your brain to your heart, lungs and digestive tract.
The vagus nerve’s job is to regulate your parasympathetic nervous system. This is one half of your autonomic nervous system, all of which works without your needing to think about it. The parasympathetic functions are often characterized as rest-and-digest.
For example, in the heart, the vagus nerve releases a neurotransmitter called acetylcholine. Acetylcholine binds to special pacemaker cells to slow the heart rate down. Behaviors such as deep, slow breathing during yoga try to increase parasympathetic activity, slowing the heart and leading to a more relaxed state.
While relaxation is a good thing, slowing the heart down too much is not – as when it leads to a brief loss of consciousness. You need your heart rate to be a certain number of beats per minute in order to contribute adequately to your overall blood pressure.
The other half of your autonomic nervous system is the sympathetic nervous system. It’s responsible for the fight-or-flight response, the functional opposite of the parasympathetic nervous system. The sympathetic nervous system makes sure the small blood vessels in your body’s tissue maintain a baseline level of constriction. This resistance as blood flows through all your narrow blood vessels contributes to sufficient blood pressure for the whole system.
An increase in parasympathetic activity reverses this resistance, allowing blood to linger in the peripheral tissues rather than heading to the heart and brain. A lack of resistance, along with the lowered heart rate, causes a dramatic decrease in blood pressure.
And you’ve fainted – or more technically, experienced a neurocardiogenic syncope. While sometimes embarrassing, it’s fairly common and, in itself, not overly dangerous.
When a sight or sound is the trigger
The physical causes of fainting make logical sense. But there’s some psychology involved here, too. Think about someone who faints at the sight of blood. What’s going on there that can lead to this overactive vasovagal response?
Typically, when the body senses an initial stress – like seeing blood – it triggers a fear-filled response that increases sympathetic nervous system activity and the heart rate rises. The body reflexively compensates by increasing parasympathetic activity to slow the heart rate back toward normal. But if the parasympathetic system overcompensates and lowers the heart rate too much, blood pressure can decrease too much, the brain gets less oxygen … and you lose consciousness.
 Even the thought of blood can trigger some people to faint. Pressmaster/Shutterstock.com
Even the thought of blood can trigger some people to faint. Pressmaster/Shutterstock.com
Whatever the cause of the fainting spell, the loss of consciousness is typically brief; most people will come to immediately after hitting the floor or even slumping over in a chair. In this sense, some researchers have suggested that fainting is protective. Once lying down, there’s no longer a gravitational challenge in delivering blood to the brain – it’s now at the same level as the heart. And, if one were actually hemorrhaging, or losing blood, the lying down, motionless posture would preserve blood and reduce further injury.
The process of going from standing or sitting to lying on the floor is actually one of the more dangerous aspects of fainting, though. Individuals may hit their head or other body parts on the way down, causing injury.
The idea that fainting may be related to the potential for blood loss, rather than a response to needles themselves or a medical procedure in general, has been a topic of recent investigations. In one study of healthy people, watching a video of a blood draw led to slightly greater activation of the parasympathetic response than did watching a very similar video of an injection, suggesting there is something special about the blood itself.
This same research group has also shown that, if a person believes they are able to stop the procedure at any time, vasovagal symptoms can be minimized. This suggests the feeling of fear or lack of control may contribute to the severity of people’s responses.
Minimize the likelihood
All the different causes for fainting and all the various reasons one person might be predisposed remain unclear, although it’s well accepted by scientists that females are more likely to experience syncope.
What is clear are some of the strategies that can help prevent fainting.
- Undergo procedures lying down in the supine position. If you do feel faint, bend your knees or elevate your legs to facilitate blood flow to your brain.
- Contract the muscles in your arms and legs to help move blood back to the heart and brain.
- Stay well hydrated to maintain sufficient overall blood volume.
Remember that an occasional episode of vasovagal syncope is likely not of concern, as long as you haven’t been injured in the process. But if fainting occurs repeatedly, it’s worth scheduling a medical exam.
About The Author
Anne R. Crecelius, Associate Professor of Health and Sport Science, University of Dayton
This article is republished from The Conversation under a Creative Commons license. Read the original article.
books_health









